REGULATORY ALERT
Georgia’s $25 Million Parity Penalty: A New Era of Accountability for Payers?
Regulators are moving from policy review to operational audits. Georgia’s $25M fine isn't just a penalty; it’s a blueprint for future state enforcement.
On January 13, 2026, Georgia’s Insurance and Safety Fire Commissioner John F. King issued nearly $25 million in fines against an array of health insurers for violations of the state’s Mental Health Parity Act, a statute that aligns with the federal Mental Health Parity and Addiction Equity Act (MHPAEA) in requiring that mental health and substance use disorder benefits be provided on terms no more restrictive than medical and surgical benefits.1
For payers, whether they’re a large national carrier or a regional plan, this enforcement action exposes a growing problem: mental health parity is no longer being evaluated on the policy level, but at the operational level. Regulators are applying more rigorous audit standards, expanding scrutiny of non-qualitative treatment limitations (NQTLs), and treating inconsistencies in administration as material compliance failures. The result is a sharply elevated regulatory and financial risk environment. Understanding how parity audits are conducted, where payers are most exposed, and how enforcement expectations are evolving is now essential to mitigating that risk.
What “Mental Health Parity” Actually Means
Mental health parity requires that mental health and substance use disorder benefits be administered no more restrictively than medical and surgical benefits. In practice, this extends beyond written plan policies to include utilization management, prior authorization criteria, medical necessity standards, claims processing, and other non-quantitative treatment limitations. Georgia’s audit took into account more than the theoretical parity in plan’s policies and procedures; it reviewed how benefits functioned in real-world operations.
Why Georgia’s Enforcement Matters
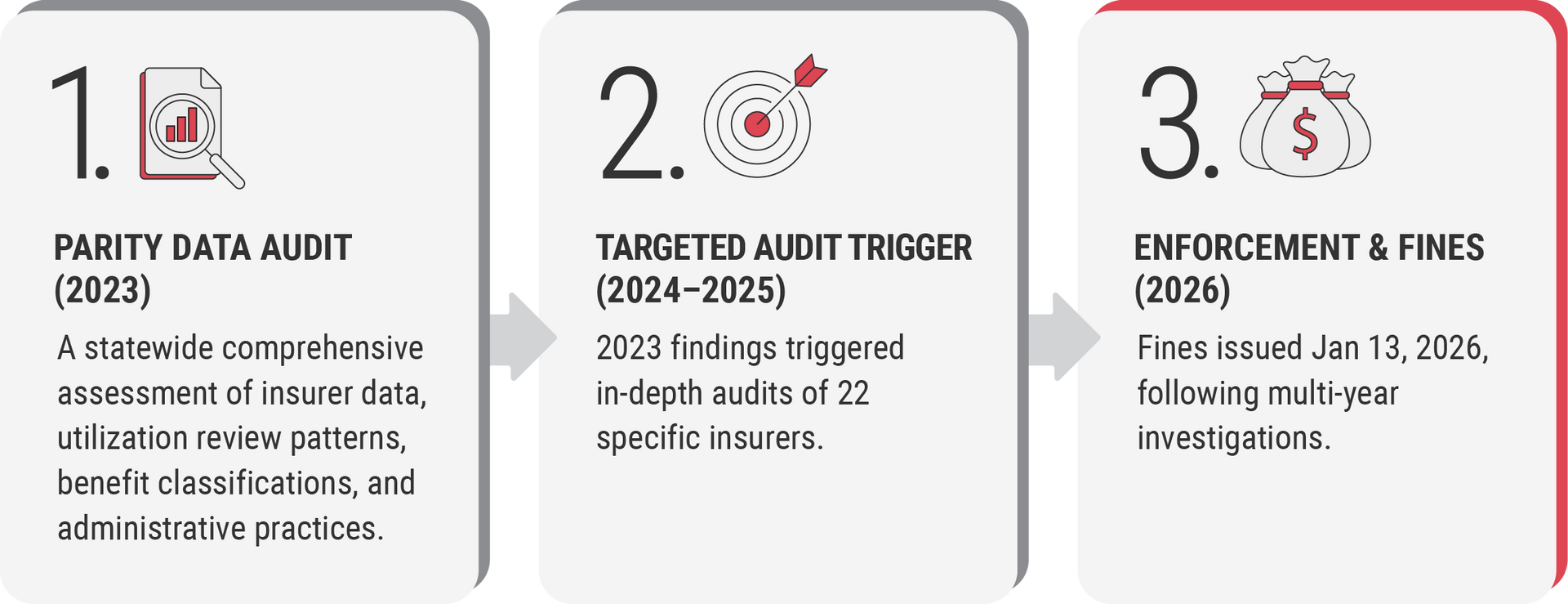
Historically, parity compliance has been considered a compliance checkbox by most risk management teams. The Georgia action, however, underscores that regulators can (and will) use market conduct exams to dig more deeply into products, processes, and internal controls. These exams began with a 2023 statewide parity data reporting that assessed insurer data, utilization review patterns, benefit classifications, and administrative practices. Findings from that report triggered in-depth audits of 22 insurers, culminating in the $25 million fines.
Parity Audits: From Concept to Intensive Scrutiny
Parity audits, especially state market conduct examinations, are comprehensive and data-intensive. They typically include:
- Comparative analysis of mental health benefits versus medical/surgical benefits, not just on paper, but in practice
- Review of NQTLs, such as prior authorization criteria, utilization management protocols, medical necessity definitions, and the clinical review process
- Claims processing practices, including consistency of decisions and documentation
- Internal governance and compliance infrastructure around parity
Georgia’s market conduct exams spanned months to years of data and pulled millions of data points to identify violations: a model that could increasingly inform other states’ enforcement approaches.
Operational Impacts on Payers
For payers, these audits have immediate and long-term operational implications:
Analytics and Data Preparedness: Insurers must build robust testing capabilities that can generate defensible comparative analysis of mental health and medical benefits. This includes aligning data structures to produce parity-relevant metrics on utilization, authorizations, denials, and appeals.
NQTL Documentation and Rationale: Payers need to make sure that they aren’t just verifying that limits match, but that the rules are applied equitably. A utilization review threshold or prior authorization rule that’s used more stringently for behavioral health services than medical services, even if both policies are written identically, may be flagged as a parity violation if the rationale isn’t documented and justified with evidence such as documented clinical logic and internal oversight.
Governance and Compliance Programs: Payers need to elevate parity compliance from a legal requirement to a core enterprise risk. That means formal governance structures, regular internal audits, and transparency into parity metrics. Documentation of compliance strategy is as crucial as operational compliance itself.
Corrective Actions and Regulatory Dialogue: Payers should be ready for a dialogue with regulators, not one-time data submissions. In Georgia’s process, insurers were required to develop corrective action plans with state regulators. Failure to implement those corrective actions or demonstrate timely compliance can trigger further penalties or more intensive oversight.
Strategic Risk and Financial Planning
While Georgia’s fines represent immediate financial penalties, the strategic cost of insufficient parity compliance can ripple further, causing:
- Increased compliance costs: Expect investment in data infrastructure, expertise in parity analytics, and possibly external audit support.
- Liability exposure: Beyond state fines, parity violations can lead to federal scrutiny, class actions, or civil penalties under MHPAEA enforcement by federal agencies
- Reputation risks: Public enforcement actions often draw media attention and can influence consumer and employer perceptions of payer reliability.
Broader Regulatory Momentum
Georgia isn’t alone. Nationally, regulators at the federal level are increasingly emphasizing that parity isn’t a theoretical entitlement but a practical compliance obligation. The U.S. Departments of Labor, Health and Human Services, and Treasury all finalized updated parity rules with enhanced expectations for NQTL comparative analysis, requiring payers to prove that mental health coverage is actually on par with medical/surgical benefits.2
States are also stepping into the fray. Georgia’s actions may embolden other states to pursue similar market conduct exams of insurers within their states.
For payers, the lesson is clear: parity compliance is no longer just an item on the regulatory to-do list. It is now a strategic, operational, and financial priority that touches products, clinical policy, provider relations, and analytics.
Insurers that treat parity compliance as a checkbox risk misalignment with evolving regulatory expectations: an alignment that Georgia’s action shows now include punitive measures when practice diverges from policy.
Georgia’s nearly $25 million enforcement action is an early indicator that markets are entering a compliance era where parity audits are not theoretical, and non-compliance carries real consequences. This is precisely the moment when a clear 90-day action plan matters—one that prioritizes rapid parity risk assessment, validates NQTL application in practice, and establishes audit readiness if scrutiny comes sooner than expected.
References:
- Georgia Insurance Commissioner Fines Insurance Companies Upwards of $25 Million for Mental Health Parity Violations; The Georgia Virtue; January 13, 2026
- Mental Health Parity Rule: Industry Reactions and Implications; Avalere Health Advisory; October 18, 2024